This article is a standalone piece and also kind of serves as the third piece of ‘The brain, movement and pain’ series already released earlier on this blog site.
This follows the loose ‘brain model’ of
Patterns
Perception
Prediction
In this model the brain uses stored neural patterns that are triggered by and compared with feedback to make a prediction of an outcome. Although we may not need any specific feedback to make a prediction, just stored memories.
This piece focuses on the brains prediction to create an output and/or action. In our opinion movement and pain would fall into these categories.
This piece focuses more on pain than movement. Pain is certainly not an area of Cor-kinetic’s expertise but a definite area of interest.
The problems may occur when the prediction of the brain is not a beneficial one. This could be when the prediction of danger or threat is not in proportion to the actual reality of threat to the tissue, especially after previous pain or injury. Pain can be the result of this prediction to limit possible damage even after the state of the tissue has improved.
This is by no means a comprehensive look at the pain experience, just some thoughts. Pain is caused and modulated by many contributing factors often with no single factor to blame in isolation.
Pain
Pain is an exceptionally tricky subject. We know much more about pain than we really know what to do about it and the fact that it is so prevalent provides a significant problem.
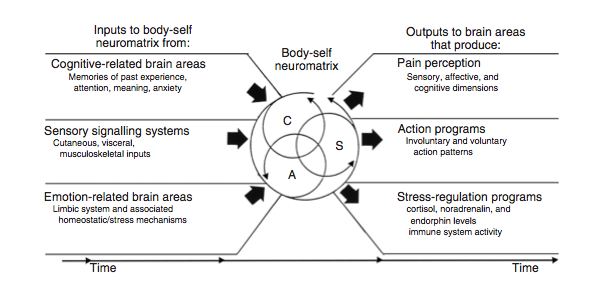
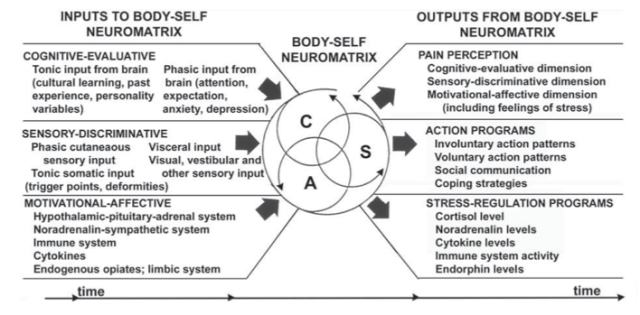
Often reconceptualizing a problem can help us change our approach as a few enlightened souls have blazed a trail in the understanding of pain. They have provided new perspectives on the previous Cartesian view that had or could be argued still is, the dominant understanding of the pain process. One such pioneer would be Ronald Melzack and his seminal “neuromatrix’ model. *Click Here* for full paper
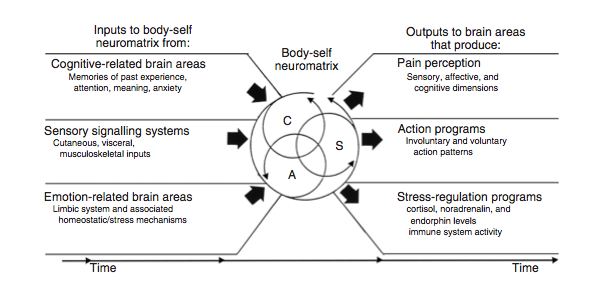 (Updated model from, Pain, Melzack and Katz 2013)
(Updated model from, Pain, Melzack and Katz 2013)
It would seem the key to a modern understanding of pain is that it is an output of the brain rather than an input from the body. This starts to separate the connection between damage to a tissue and amount of pain experienced or even nociceptor activity and the pain experienced. The central processing of stimulus, potentially painful or not, within the brain is key to the level of pain experienced by the individual. In fact we may not need any stimulus from the body at all to create pain as we will further discuss.
Lorimer Moseley explains this far more eloquently in, Reconceptualising pain according to modern pain science. Physical Therapy Reviews (2007)
“it is clear that experimental studies do not show an isomorphic relationship between pain and nociceptor activity, nor between pain and the state of the tissues. Rather, they show a variable relationship that is modulated by many factors”
Pain and pathology
The fact that pain can persist many months or years after an injury also confounds the current opinion that pain levels correlates with state of the tissue. This also questions the constant search for pathology to link with the current pain state of the patient.
Boden et al (1990) performed, Abnormal magnetic-resonance scans of the lumbar spine in asymptomatic subjects. A prospective investigation, that is scans on individuals with no pain. They found that one-third displayed ‘substantial abnormality’. This raised to 57% for those over sixty. More surprisingly 35% of the subjects between 20 & 39 years old had bulging or degeneration of a lumbar disc.
Borenstein (2001) also looked at MRI as a predictor of lower back pain of asymptomatic individuals. “The value of magnetic resonance imaging of the lumbar spine to predict low-back pain in asymptomatic subjects : a seven-year follow-up study.”
They found:
“The findings on magnetic resonance scans were not predictive of the development or duration of low-back pain. Individuals with the longest duration of low-back pain did not have the greatest degree of anatomical abnormality on the original, 1989 scans”
A recent study by Graves et al (2012), ‘Early imaging for acute low back pain: one-year health and disability outcomes among Washington State workers’, actually found that:
“Among workers with LBP, early MRI is not associated with better health outcomes and is associated with increased likelihood of disability and its duration”
It lead to a 2-fold increase in the liklehood of work disability benefit 1 year later.
Surgical procedures in response to disc herniation only provides complete relief from pain and sciatic symptoms in 60% of cases. Patients are also rarely helped by vertebrae fusion to provide support for the back. (Melzack, Full article here – Pain 2013)
This highlights the variable relationship with pain and tissue state as discussed by Moseley. An early correlation with tissue state did not lead to a better outcome. Did the link to’pathology’ in fact increase the duration of the pain experience? Again this widens a predictable link between tissue state and pain and also brings into play the patients cognitive evaluation of the situation.
Although we have tried to find many biomechanical or anatomical ‘flaws’ or ‘anomalies’ within the human condition to blame or attempt to predict for various chronic pain. It has proved an elusive game that has not been reliably supported by high quality research and still remains rife with opinion presented as fact.
Pain as an output
To widen the gap between pain and the state of the tissue and make us further evaluate the idea of pain as an output of the brain we must start to look at pain that cannot involve any input from the body. A perfect example would be ‘phantom limb’ pain.
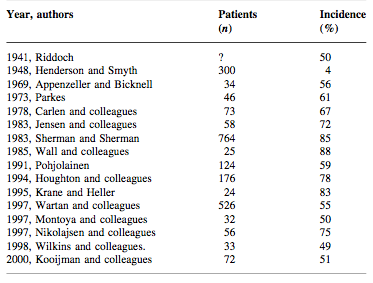
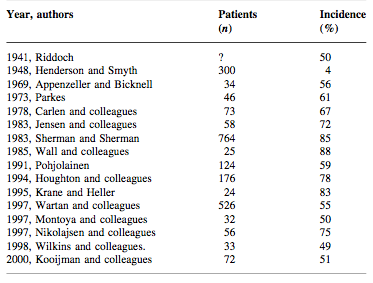
‘Phantom limb’ is when amputee patients still get pain in their limb that has been amputated. It is not an uncommon experience. Nikolajsen & Jenson in “Phantom limb pain” (2001) found more recent studies reported incidences of phantom limb pain of 60 -80%.
Melzack and Katz in their article “Pain” (2013) when discussing phantom limbs state:
“all the qualities of experience we normally feel from the body, including pain, are also felt in the absence of inputs from the body; from this we may conclude that the origins of the patterns of experience lie in neural networks in the brain; stimuli may trigger the patterns but do not produce them”
Macabe et al (2006) in “Simulating sensory–motor incongruence in healthy volunteers: implications for a cortical model of pain” looked at
“Conditions that occur in the absence of a discernible peripheral causal pathology or appear disproportionate to the size of the injury”
such as
“Repetitive strain injury, complex regional pain syndrome-type 1 (CRPS), fibromyalgia, focal hand dystonia and phantom limb pain”
They sought to induce pain in health individuals through motor-sensory central nervous processing. They found:
“Twenty-seven subjects (66%) reported at least one anomalous sensory symptom at some stage in the protocol despite no peripheral nociceptive input.”
Both of the examples above bring into question the current hegemony of pain only stemming from damaged tissue, pathology or structural abnormality. In fact we see pain in these examples without any ‘noxious stimulus’ in some cases without any stimulus or input to the brain at all.
Melzack and Katz in their article ‘Pain’ add:
“In short, phantom limbs are a mystery only if we assume the body sends sensory messages to a passively receiving brain. Phantoms become comprehensible once we recognize that the brain generates the experience of the body. Sensory inputs merely modulate that experience; they do not directly cause it”
Pain as a prediction
So we come to the real subject of the piece. That is introducing pain as a ‘prediction’ of the brain that requires no input from the periphery. This can be why pain can persist long after tissue may heal or in the absence of pathology, and why some people despite MRI findings that we would associate with pain, experience little or no pain.
In Norman Doidge’s book “The brain that changes itself”, Doidge talks to the Indian neuroscientist Ramachandran who has been instrumental in understanding neuroplasticity and phantom limb pain.
Ramachandran discusses chronic pain patients and his belief “motor commands are wired into the pain system” or possibly this could be pain association is wired into the motor program (neurosignature/tag) for certain movements. This may happen after an injury has occurred and to protect the injured tissue the motor command changes. Motor changes in response to pain or injury has also been discussed by Hodges in his ‘Moving differently in pain’ (2010) article.
“When we guard we prevent our muscles from moving and aggravating our injury, if we had to remind ourselves consciously not to move, we’d become exhausted and slip up, hurt ourselves and cause pain” (Ramachandran)
“The brain that changes itself” Norman Doidge. Penguin, 2007, p193.
This causes a neuroplastic change within the functional organization of the brain, creating a ‘”pathological form of guarding”
He goes on to say
“now suppose, thought Ramachandran, the brain preempts the mistaken movement by triggering pain before the movement takes place, between the time when the motor centre issues a command to move and the time when the move is performed” (Ramachandran)
“The brain that changes itself” Norman Doidge. Penguin, 2007, p193.
Understanding pain as an output is vital to this viewpoint. ‘Guarding’ of a movement in the author’s opinion can be both a motor and a pain output. The body can choose to limit movement both through the range or direction of a movement and a pain response.
Where this becomes a problem is once the tissue has healed.
“Ramachandran came to believe that in these chronic pain patients the pain command got wired into the pain system, so that even though the limb had healed, when the brain sent out a motor command to move the arm, it still triggered pain”
The brain still sees the body part as a problem. Taking this one step further we could start to get pain or discomfort with the thought of moving the affected body part or even discussing it. It would depend on the ‘wiring’ of pain into the many neural patterns involved with painful area in multiple parts of the brain.
One of Lorimer Moseley’s key points in “Reconceptualising pain according to modern pain science“ is
“iv. that pain can be conceptualised as a conscious correlate of the implicit perception that tissue is in danger”
Here we see a consensus on the state of the tissue being unimportant compared to the perception of the state of the tissue or the perception of the tissue being endangered.
This perception could be based on previous events that have occurred to the tissue, such as injury or pain, or movement that the brain may feel is endangering to the tissue. This opens up a whole world of possibilities of previous movement/pain experiences or prediction of future experience having an effect on the pain output from the brain. The damage to the tissue at the site of pain experienced as a cause or link to pathology becoming further removed from the pain experienced. Any correlation further diminishing as more time elapses (Moseley 2007) However we must be mindful that the pain experienced is still very real to the person experiencing it.
Memory-prediction model
One theory of how the brain works is via a memory-prediction model. It is further discussed in this article.
The brain, movement and pain. Sportex July 2013
Faced with so many variables and unable to process them all the brain uses prediction based on previous events and learning experiences. Bayesian probability theory may give some insight into how this model may work.
“To evaluate the probability of a hypothesis, the Bayesian probabilist specifies some prior probability, which is then updated in the light of new, relevant data“
Bayesian probablility. Wikipedia.
An example of this could be that you hear a song on the radio you know and are singing along. You use your prior memory of the song to predict the upcoming words. We see the same thing in game shows when we fill in the missing letters to a word or fill in the missing word to complete a well-known phrase. The examples available to use to explain the memory-prediction model are countless.
We see this neural process at a base level with rats in response to a reward or sanction associated with pressing a button.
In this way we can start to see a link between past events and the current prediction of threat or danger to a tissue or tissue state. Especially with a memorable event such as pain.
The prediction is influenced by what has happened in the past. Both on a direct level in terms of storage and recall of specific actions or outputs and also in the overall processing of input and subsequent output commands through our individual ‘neuromatrix’ shaped by both genetic and learned factors.

If we perceive the state of a tissue, regardless of the actual state, as damaged or likely to be further damaged by a motor action, a prediction of a future tissue state, then a pain output could be used to prevent the motor action or a pain association used as an efficient way to limit or modify movement at a motor planning stage.
The problem here maybe that it is not the painful movement or pathology (if present or relevant) is the real problem. Instead it is the perception and subsequent prediction of further damage by the brain. It is much harder to change a learned response. In fact Ramachandran calls this ‘learned pain’. The pain is a habit and as we all know habits can be hard to break.
Pain ‘memories’
Melzack discusses ‘somatic memories’ in his paper, “Pain ‘memories’ in phantom limbs: review and clinical observations” Even though the limb is no longer present, pre amputation pain persists in the ‘phantom limb’.
Melzack Says
“The results suggest that somatosensory inputs of sufficient intensity and duration can produce lasting changes in central neural structures”
The injuries are varied encompassing:
“cutaneous lesions, deep tissue injuries, bone and joint pain and painful pre-amputation postures”
The pain does not exist within the periphery, it cannot. Instead neuroplastically altering the brain in the specific representations relating to the limb. The question is does this happen in less extreme examples than complete deafferentation?
David Butler in “The sensitive nervous system”, NOIgroup Publications, 2000, says:
“Overuse, lack of use, minor injuries and associated cognitions will also alter representations. Amputation simply serves as a dramatic example”
Here we see previous pain experiences affecting future pain experiences. On a less extreme level than complete deafferentation do we regularly see our pain ‘memories’ neuroplastically reorganizing our brain, therefore altering its future perceptions and subsequent predictions of threat to a tissue? The brain output may range from minor alterations in movement right up to debilitating chronic pain.
The ‘’forward’ model
A predictive model has also been hypothesized in motor control theory. The ‘forward’ model of motor control.
Fleischer discusses the ‘forward model’ in his paper “Neural Correlates of Anticipation in Cerebellum, Basal Ganglia, and Hippocampus”
“A forward model provides the nervous system with a prediction of what the body state will be like in the near future”
He adds
“Optimal motor control theory requires the presence of a forward computation of what the effect of a motor command will be given the current state and motor commands”
And
“Alternatively, a forward model can allow the production of movements that are faster than using only feedback control”
It is important to appreciate the Cerebellums link with the cerebral cortex where our somatotopic representations are stored and the constant information flow between the two areas when moving. We compare intended movement from the motor areas with reported movement from the periphery using the information to alter motor commands to achieve the desired task.
Here again we are seeing the implications of feed forward model rather than a feedback. A need to be able to predict what will happen that can only be based on previous experience. In both pain and movement control often the feedback model rules such as in the force-based model of biomechanics or Cartesian view of pain.
Implications for biomechanics
A question we have to ask ourselves is the implication for a structural biomechanical model. A structural ‘anomaly’ may not be able to alter a movement in the predictable way we anticipate when we factor in a ‘forward’ model of motor control. If we consider pain as a prediction and associated to a motor command rather than as a result of the movement and actual affect on the tissue it must force us to possibly rethink the biomechanical/Cartesian feedback perspective. A question is “has the movement caused pain or pain altered the movement?” Changing subconscious perception of the tissue maybe most important rather than specific movements deemed as abnormal or damaging by the practitioner.
Better representations, better predictions?
Our neural structures and their organization appears to be important in how we predict future events if we include the memory-prediction model in our considerations.
Our somatotopic representations have been implicated in chronic pain states by Butler, Moseley, Flor and Ramashandran amongst others.
Moseley and Flor in “Targeting Cortical Representations in the Treatment of Chronic Pain: A Review” (2012) explain:
“A large body of evidence shows that chronic pain is associated with disruption of a range of body-related cortical representations. There is some evidence that this disruption contributes to, or maintains, chronic pain”
We may use these representations to predict future levels of threat or danger to a tissue and significant changes have been documented in these areas with people in chronic pain. Has pain altered the representation or has the altered representation contributed to pain? This is a tough question to answer but both scenarios must be considered.
Targeting cortical representations has been proposed and implemented by Moseley and Flor and by the NOI group with their graded motor imagery program http://www.gradedmotorimagery.com/

Falla et al in “The role of motor learning and neuroplasticity in designing rehabilitation approaches for musculoskeletal pain disorders” (2010) state:
“In novel motor-skill acquisition, cortical neuroplastic changes are often accompanied by behavior deemed to be advantageous, such as an increase in motor performance”
They add
“Rehabilitation efforts that attempt to maxamise the extent of cortical neuroplastic changes stand to provide the greatest potential for rehabilitation success”
Moseley and Flor also add
“Treatments that target sensory and cognitive representations using sensory and motor strategies show clear functional and symptomatic benefits”
Breaking the cycle
In our opinion it may be breaking the prediction that helps change a persistent pain response although specific ‘hows’ is not really the focus of this piece. This could involve becoming aware of behaviors, emotions and movement strategies to break the subconscious ingrained output associated with pain.
This could be as simple as consciously relaxing before moving in some cases. Anecdotal success has been gained via using this method. Just being able to modify pain through simple sequential changes to a motor action may give the patient back some level of internal locus of control and have an effect on their emotional state as well as altering prediction of threat.
Pain education and the bio-psycho -social model may also have implications for changing prediction or perception of pain and threat. Helping reevaluate the link between what the patient is experiencing and the actual harm to their bodies.
Subtle shifts in context may have an affect on the specific motor command that has a pain component ‘wired’ in. This could be body position, location or emotional state.
Non-painful movement as close to the painful movement as possible may allow us to keep or build movement confidence without reinforcing pain association. Subtle changes in limb position may alter the pain response and reduce protective mechanisms associated with movement and pain. This may need to be regressed to any non-painful/threatening movement of the afflicted area depending on the severity of the pain output.
Conclusion
It is important to start to disassociate pain from tissue state, pathology, nociception and biomechanics. Pain is an output of the brain that can occur without any input from the body. This however does not mean any of these components cannot cause pain but pain is certainly not exclusive to them, as many seem to currently believe.
A prediction of pain based on prior learned experiences that may change the functional organization of the brain may create a feed forward model of pain during movement. This can also be modulated by many factors such as stress and illness affecting our individual ‘neuromatix’ and amplifying the pain experience.
Targeting our cortical representations may enable us to make different, hopefully better, and long lasting change in predictions that don’t involve protecting perceived threat to tissue via limiting movement or increasing pain output. This could be done through the visual system & imagery, motor skills and subtly altering the context of a given pain situation.
 Functional Rehab Essentials for the Fit Pro
Functional Rehab Essentials for the Fit Pro